So just what is a comorbidity and why is it important to an individual with a hypothalamic hamartoma (HH)?
In medicine, a comorbidity is defined as a condition or symptom that occurs, or is seen more frequently with, a separate primary medical condition.
In the case of epilepsy, common comorbidities include cognitive decline, memory loss, depression and anxiety. And like epilepsy, HH treatment focus can often be more on seizure control or seizure freedom. While this is indeed a worthwhile goal – it may not be possible for all. What about the wide range of other devastating symptoms that may also be having a huge negative impact on an individual’s quality of life? For some, in fact, other symptoms can be harder for an individual or family to manage than seizures themselves.
In an article titled Epilepsy and Comorbidities, Dr. Nikesh Ardeshna states “…certain additional comorbidities and associated medical conditions are seen more frequently in patients with epilepsy, compared with the general population, and these comorbidities require evaluation and treatment.“ He goes on to say “These comorbidities have garnered more attention over the last few years not only because patients are reporting these symptoms more frequently, but also because these symptoms, in addition to seizures, can significantly affect a patient’s quality of life. This influence, in turn, has led to more research and literature documenting these comorbid conditions. At times, the conditions’ impact on quality of life can be greater than the impact of the epilepsy itself.”
But what are the comorbidities, or other conditions, that may be associated with having an HH, with or without epilepsy? For many individuals with HH and epilepsy, members of the medical community in general can be quick to say “I don’t know if what you are experiencing has anything to do with HH!” or “I don’t know what that is, probably something to do with the HH – but I don’t know what to do about it.” or even perhaps “It is an HH. You just have surgery to remove it and everything else will go away”. So, which is it?
Hope for HH has taken on this topic as one of our top issues for 2019. In the upcoming blogs, I will present some of the most commonly reported symptoms by our HH Community. The goal is to generate discussion and compile a comprehensive list of symptoms that may be either undiagnosed or under-diagnosed, based on input from individuals with HH and/or their caregivers. In the coming months, we will circulate a survey to the HH Community in order to gather data, in as scientific a format as possible. We plan on presenting the data to experts, from a broad range of specialties, that will be attending our 4th International HH Symposium in Washington DC this Fall. There, we hope to open up the discussion and facilitate the development of an internationally recognized HH Syndrome definition. This all-inclusive description would help clinicians establish more comprehensive treatment protocols and encourage researchers from more diverse specialties to get involved. This could potentially improve overall treatment outcomes and ultimately, improve the quality of life for individuals of all ages affected by the truly complex condition that is HH.
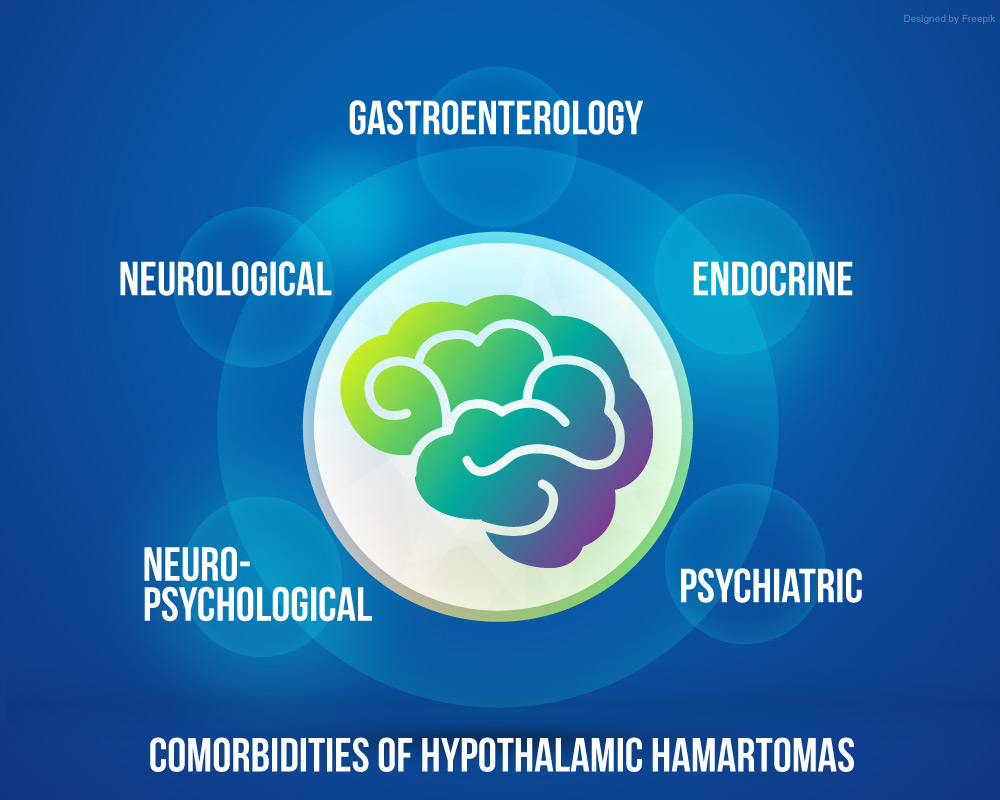
Some of the functional areas we will be exploring will include:
- Psychiatric – Behavior, mental health issues, depression, anxiety
- Endocrine – Growth issues, thyroid, hormones, Hypothalamic Obesity
- Neuropsychological – Memory, cognitive, executive function
- Gastroenterology – Intestinal issues
- Neurological – Seizures, headaches, sleep issues
Our goal is to be the voice of this community. We hope everyone will participate in the initial discussion and the upcoming survey. You can help us educate the medical professionals involved in our care. HH may indeed be rare, but it could and should be much better defined.
Resources:
Clinical Topics – Epilepsy and Comorbidities. Article by Nikesh Ardeshna, MD medical Director of Adult Epilepsy Services at Royal Oak Hospital, Beaumont Health System, in Royal Oak, Michigan.





