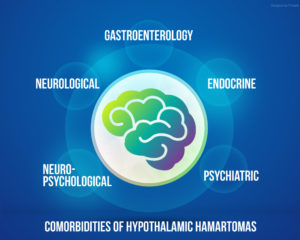
In my last blog, I introduced the concept of comorbidities and hypothalamic hamartomas (HH). If you happened to miss that blog, you can read it here.
In that blog, I noted that in medicine, a comorbidity is defined as a condition or symptom that occurs, or is seen more frequently with, a separate primary medical condition. Today, we are going to discuss the most commonly reported endocrine issues associated with hypothalamic hamartomas.
It is important to distinguish comorbidities (or symptoms) as those conditions present BEFORE any kind of treatment. There are MANY complications that can result AFTER surgery due to insult or injury to the hypothalamus. Those would be attributed to complications of the treatment and not comorbidities of the lesion itself.
The goal today is to learn more about the importance of the entire endocrine system and the impact an HH might have on that critical system.
A basic understanding of how the hypothalamus and pituitary gland work together in hormone regulation is important. While a challenging subject to summarize in a short blog – there are some great videos that explain the relationship quite well – in the least technical terms possible.
These are both fantastic video resources to better understand the endocrine system and the importance of the hypothalamus.
- Endocrine Control – (YouTube video by Khanacademymedicine). A bit scientific but excellent source of information for the complex endocrine patient
- 2-Minute Neuroscience: Hypothalamus & Pituitary Gland – excellent concise video on the hypothalamus and important hormones released by the pituitary gland.
You may be surprised to know the major glands of the endocrine system are the hypothalamus, pituitary, thyroid, parathyroids, adrenals, pineal body, and the reproductive organs (ovaries and testes). The pancreas is also a part of this system; it has a role in hormone production as well as in digestion.
The endocrine issue most reported by the medical community as a comorbidity of HH is Precocious Puberty. It has been stated that “on rare occasions, there can also be growth hormone deficiency, hypothyroidism, and adrenal insufficiency”. (1) Many patients and caregivers report the incidence of these and other conditions are much more common.
Other endocrine related issues reported by individuals and families include:
- Poor temperature regulation or tolerance to heat
- Excessive weight gain
- Unusual sweating (amount or side part of the body and not the other)
- Advanced bone age without precocious puberty
Are there more symptoms or conditions we have not listed? That is what we would like to understand and share with endocrinologists that are treating HH patients.
While endocrinologists with HH experience may be rare – those familiar with how a compromised hypothalamus influences the pituitary gland and hormonal balance can be worth their weight in gold. Those practitioners with experience treating individuals with pituitary tumors may be a great asset to your overall HH Team. They may be able to offer more suggestions when it comes to identifying and treating the many complex symptoms HH patients experience.
Our family consulted several endocrinologists before we found one that understood the symptoms our son had been experiencing for years. These symptoms had been dismissed as typically poor diet, laziness, or just “bad genes”. Our current endocrinologist has actually taken the lead in our discussions and has suggested which tests should be run in order to manage significant hormonal deficiencies that continue to be an issue as our son ages. This has improved our son’s quality of life significantly and restored my faith that there are still great professionals out there that are willing to listen.
Many individuals with HH ask “What is due to the HH (comorbidity) and what is a complication of surgery?” Hope for HH will be sharing a survey with our community in the next few months with the goal of identifying ALL of the comorbidities of HH and not the just ones that may be most “well-known”. Ultimately, our goal is to report both the under-diagnosed and the undiagnosed and establish a comprehensive description of the HH Syndrome.
We would love to hear from you – what has been your experience before surgery? Have you experienced unusual endocrine issues that have not been addressed or recognized by your providers? Let’s share those concerns and have them addressed for the community as a whole at the upcoming International HH Symposium for Professionals in Washington DC this Fall!
References:
(1)Epilepsia. 2017 Jun;58 Suppl 2:50-59. doi: 10.1111/epi.13756.
Hypothalamic hamartoma with epilepsy: Review of endocrine comorbidity.
Harrison VS1, Oatman O2, Kerrigan JF3.
(2)Epileptic Disord. 2003 Dec;5(4):239-47.
The endocrinology of hypothalamic hamartoma surgery for intractable epilepsy.
Freeman JL1, Zacharin M, Rosenfeld JV, Harvey AS.





