Grace Katherine Webster (2003 – 2011)
Perry and I had married in early 2002 with the hopes of beginning our family immediately. Unfortunately, we experienced two back to back miscarriages in 2002 and we felt the dreams of a family were slipping away from us. We decided to seek the help of a fertility specialist before moving forward. The doctor was able to determine that I had a slight blood clotting issue which was contributing to the miscarriages and felt it could be resolved successfully by taking a baby aspirin everyday. In April 2003, our prayers were answered when I became pregnant with Grace.
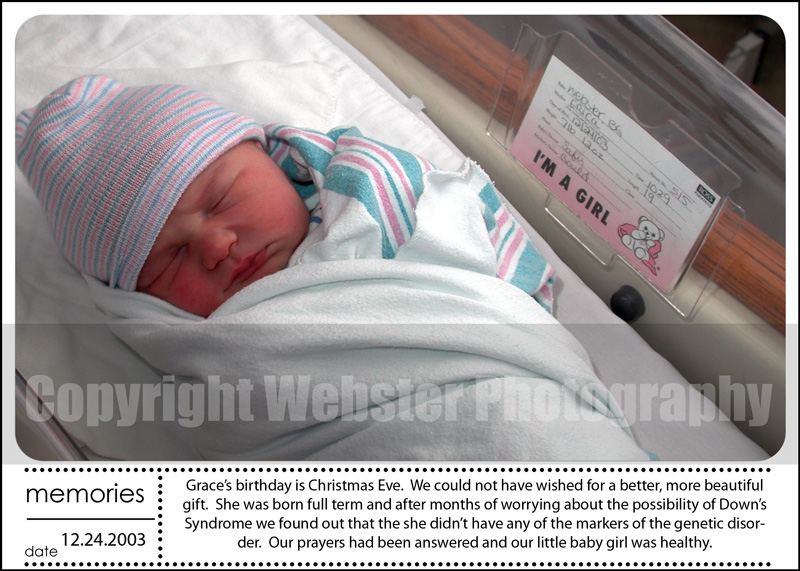
The pregnancy was watched carefully by our doctors until the first trimester ultrasounds showed a growing and healthy baby. During the second trimester, I had several routine tests completed including an AFP, which screens for potential birth defects. It was not a mandatory test, but due to our family history with spina bifida we felt it was important for us to do this for our baby. The test was routine and we honestly were not worried about the results as we didn’t expect anything to show up. Within a week or so, I received a call from my OB|GYN explaining the test came back positive for Down Syndrome. It showed a 1:10 chance for Down Syndrome, however, only an amino would be able to confirm these results. Due to our history of miscarriages, we decided not to have the amino and instead educated ourselves on Down Syndrome and prepared our world for any special needs our baby might require.
Grace Katherine Webster was born on December 24, 2003. She was absolutely angelic. Our first question after her birth was whether or not she appeared to have Down Syndrome and the doctors indicated that she did not. Grace did well the first night in the hospital and we were allowed to take our little angel home on Christmas Day. The first few weeks were difficult as Grace wasn’t gaining weight as we had hoped. We were instructed to track the ounces she was consuming and how many wet/dirty diapers she had throughout the day. It took several weeks, but things turned around and she began to put on weight.
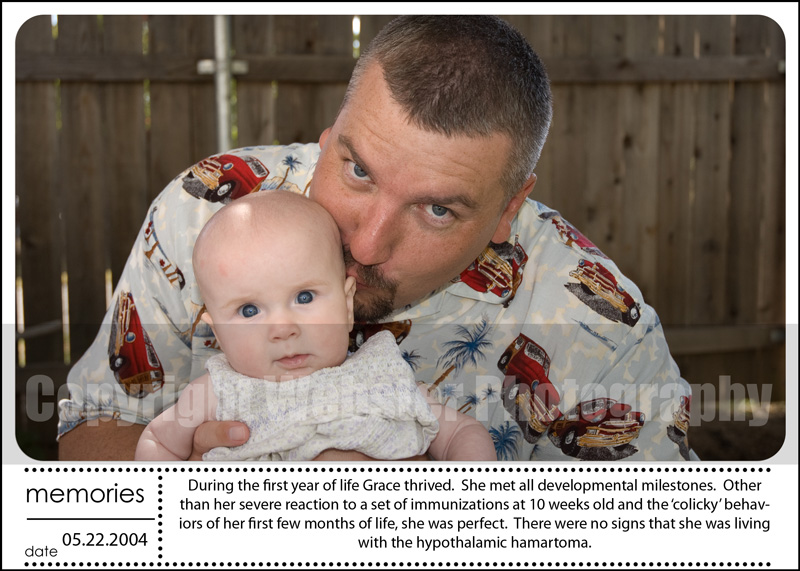
At about 10 weeks old, we took her in for a routine check up and immunizations. It was a day we will never forget. After receiving the immunizations, we went home and within a few hours Grace began to cry. She cried for nearly 21 hrs non-stop. We called the doctor and explained to him the crying and the non-stop movement of her arms and legs. He explained that she had 4 immunizations that day and apparently was having a bad reaction. He let us know that it was not uncommon and that moving forward we’d split the immunizations up over multiple days. Looking back now, we believe the stress of the immunization actually initiated 21 hours of seizures. And the weeks that followed with, what we believed was simply a colicky baby, was actually a baby experiencing seizures. But at the time, we were new parents and were confident in the care of our pediatrician.
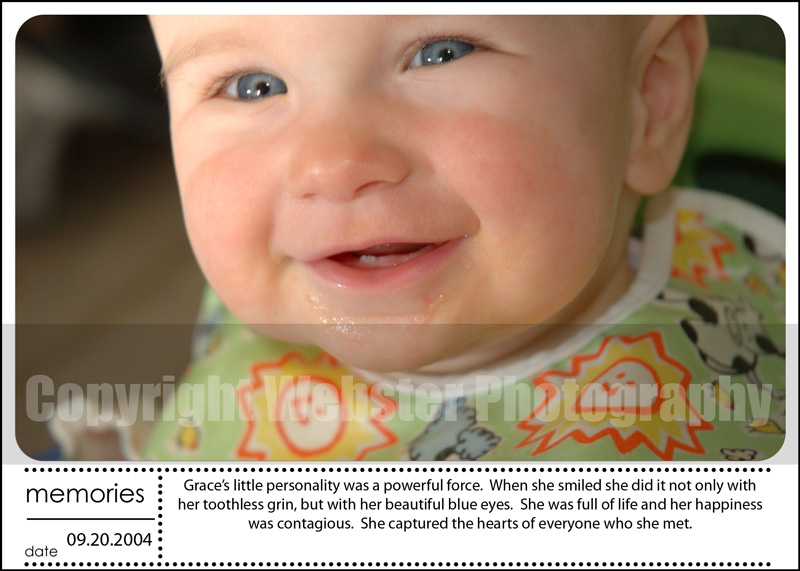
The next year was amazing. Grace eventually ‘grew out’ of the colicky stage and was one of the happiest babies I had ever seen. When she smiled, it was with her entire face, from the twinkle in her beautiful blue eyes to a little toothless grin. She could light up a room and melt hearts by her simple smile.
In late 2004, we decided to move from the Bay Area back to where Perry grew up to be close to Perry’s parents. Grace celebrated her first birthday in the new house surrounded by family. Life was good.
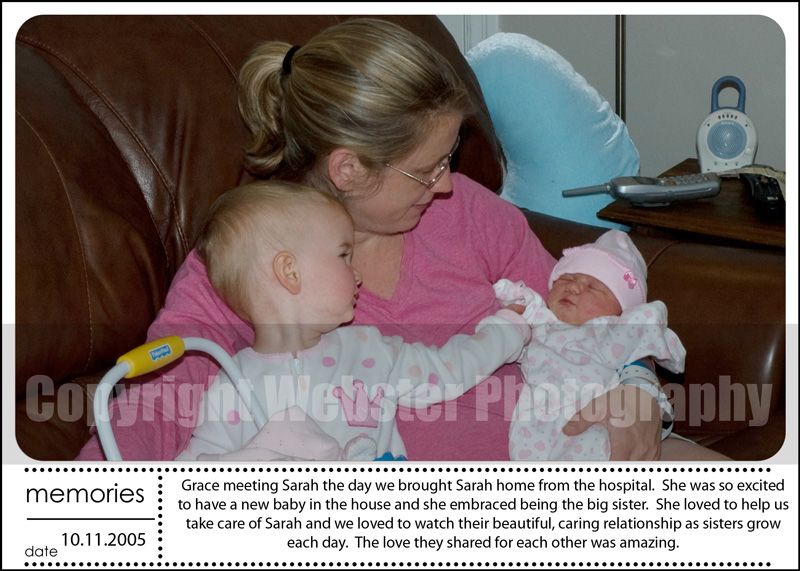
In February 2005, we found out we were expecting again. Life was just getting better by the minute.
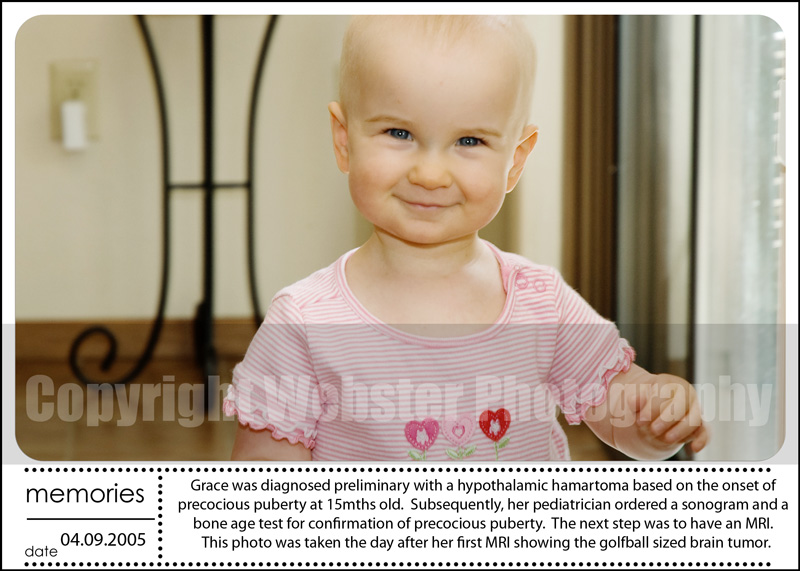
April 2005, our world would be shattered. It was an ordinary day, everything was normal. It was the afternoon and I was changing Grace’s diaper and noticed a bit of blood. It didn’t alarm me initially as we had just begun to wean her from the bottle and I figured she might have not been drinking enough fluids and had gotten a urinary tract infection. I called the doctor and she asked me to come in that afternoon. I was completely unprepared for the conversation. She examined Grace and when I asked if she thought it was a urinary tract infection, she without pause said, ‘no’. She sat down and I’ll never forget the feeling of absolute fear and helplessness I felt when she began to tell us the severity of the issue. She said, “Little girls only bleed down there for two reasons, either from sexual abuse or a brain tumor.” I felt like I had been kicked in the stomach, I couldn’t catch my breath. I knew it wasn’t sexual abuse. I worked from home and had a babysitter come to the home to watch Grace. I was never further than a room away from her. These moments were like walking through a dream.
The pediatrician sent us for a bone age test and a uterine sonogram. The bone age indicated a 2.5yrs versus her chronological age of 15 months. The sonogram showed her uterus was maturing to puberty. With this information, the doctor was confident that she indeed had a tumor and would need an MRI to confirm. This was the first time we heard the term ‘hypothalamic hamartoma’. She told us to go home and begin searching the internet for any and all information we could find. When we got home and began searching we found very little information, with the exception of a single support group and a hospital in Arizona.
Grace had an MRI within the week and it showed a huge tumor, hypothalamic hamartoma, measuring 3.6 x 3.0 x 3.0 cm. We were told this was causing the precocious puberty and the bone age issues. We were informed seizures and behavioral problems can also be a symptom, but at the time we believed she wasn’t having seizures and definitely had no behavioral problems. We felt lucky the only symptom she had were treatable through a monthly Lupron injection.
Within a couple of weeks we sent Grace’s records to Barrow Neurological Institute (BNI) for inclusion in their monthly review of new HH cases. The team reviewed and recommended no surgery as Grace was not having seizures and the precocious puberty was treatable. Again, we felt blessed our Grace had been spared the more debilitating symptoms of this condition.
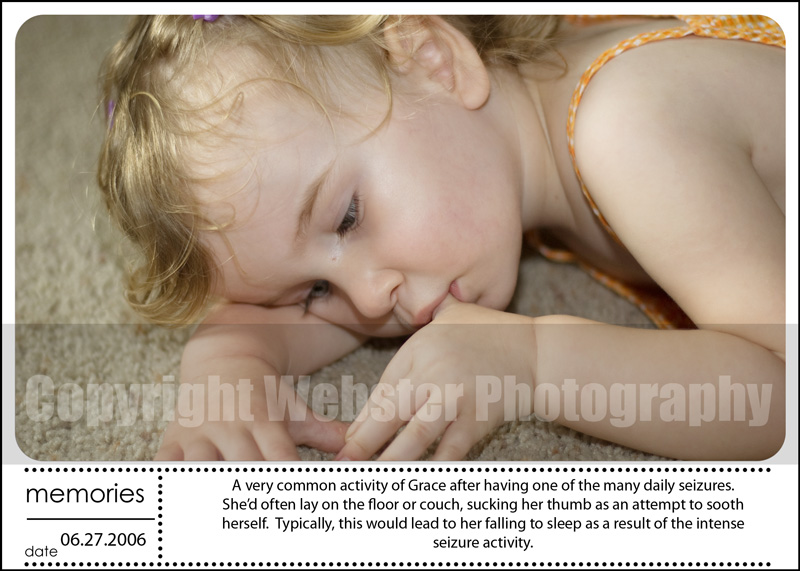
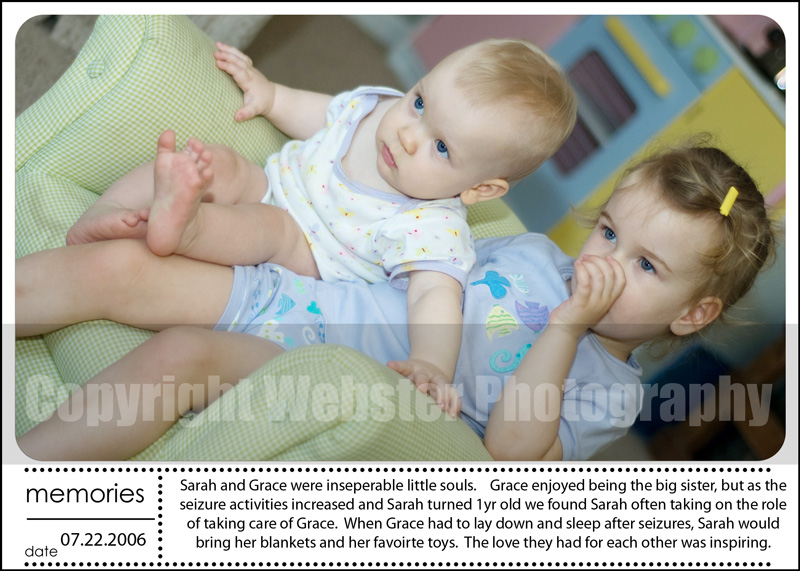
By the end of May 2005, we began to see little ‘episodes’ during the day. At the time we were terrified to actually identify them as seizures as if calling them ‘episodes’ would change them from being what they actually were, seizures. Over the next several months, the ‘episode’ frequency increased, we were beginning to see a pattern in what triggered them and noticed they seemed to be impacting Grace more and more. Grace’s seizures were triggered by any extreme onset of emotion. It could be the overstimulation of having fun and giggle, the startling effect of falling while playing, or startling of a loud noise or unexpected movement of an object near her. By the end of 2005, Grace was having more than 14 gelastic seizures per day and multiple complex partial seizures per week. Grace was put on Keppra and Tegretol and although they did not stop all the seizures, they did decrease the frequency. Her quality of life was beginning to suffer as a result. She was beginning for the first time to show the cognitive impact of the seizures, particularly in her expressive speech and was spending much of her day in ‘recovering mode’ as a result of seizures.
In April 2006, we asked BNI to re-evaluate Grace’s records as a result of the seizure increase and the cognitive decline. Due to the increase in seizure frequency, addition of seizure types, and the cognitive decline, Grace was now considered a candidate for surgery if we decided we wanted to pursue it. Perry and I felt we needed to give the medications a chance before moving forward with surgery.
Grace’s progression through the symptoms of HH continued and in July 2006, she began to have hypothalamic rages. The onset of these rages were the turning point for our family in making the decision to move forward with surgery. Grace’s quality of life had been slowly slipping away since her diagnosis, but the rages are beyond explanation. They destroy every bit of happiness and joy within the person experiencing them. They come on without warning and they leave a trail of guilt and sorrow with the person. Grace would be devastated and so incredibly remorseful afterwards. She’d tell us she didn’t know why she was doing it and that she had no control to stop. It was the most difficult aspect of HH for her and our family. She was helpless and we were equally as helpless.
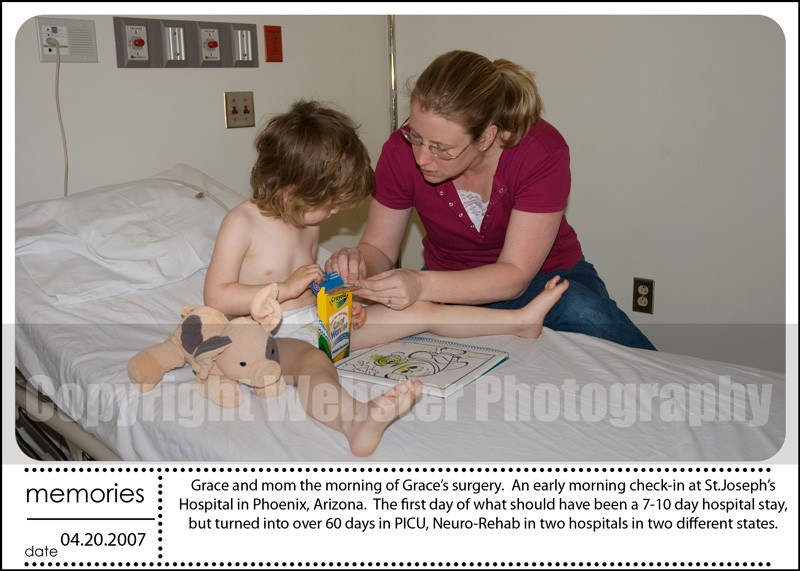
In November 2006, our family headed to Phoenix, AZ for a preliminary surgery consult with Dr.Rekate. He described the approach he’d use for resection and his recommendation was postpone the surgery for a few months until a new intra-operative MRI was up and running. He explained this new equipment would provide him and his team increased visibility during the resection. We agreed to waiting and scheduled surgery for April 2007.
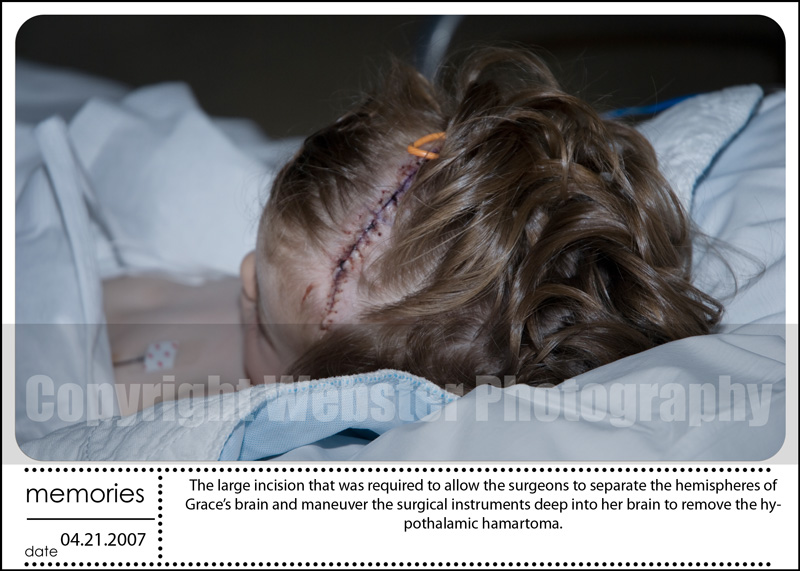
Grace went into surgery on April 20, 2007. The surgery went well and initial review indicated a 90-95% resection. We were told the following 2 days would be critical and we’d need to prepare ourselves for the recovery period.
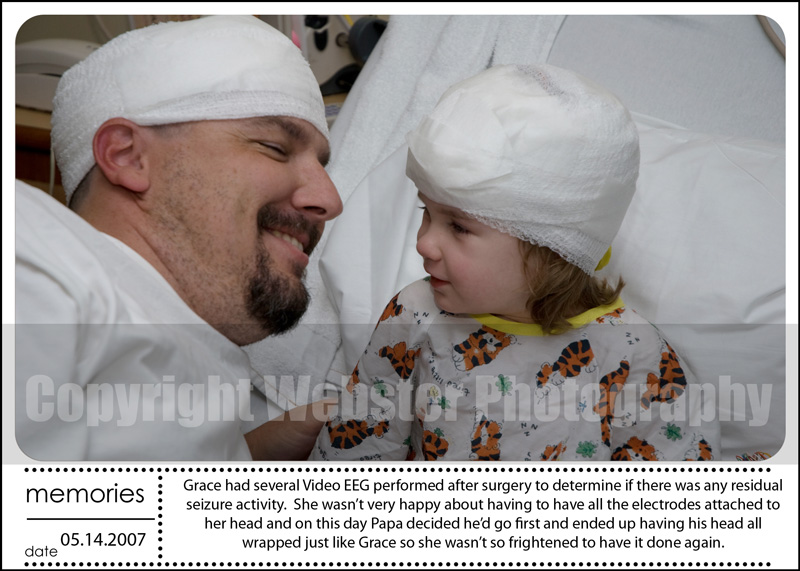
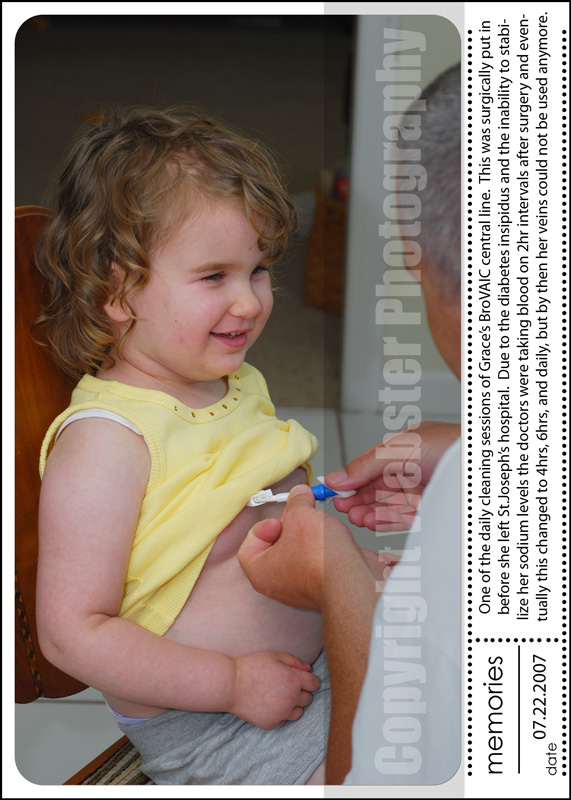
We had originally believed Grace’s time in PICU and PEDs would be a 7-10 day stay, but within the first couple of days in PICU Grace was showing signs of distress and it became evident her post-op journey would not be typical. She was running high fevers, her sodium levels wouldn’t stabilize, and on the third day she had a large seizure. Within the first week things appeared to stabilize and she was moved to the PEDs unit in hopes that she’d be ready for going home; however, within two days she experienced another large seizure and her sodium levels dropped dramatically. She was moved back to PICU for monitoring where she stayed for a month post-op before being moved to Neuro-Rehab for another 3 weeks, only then was she stabilized enough to be medically transferred to a hospital closer to home where she stayed for another week, before being released.
Grace’s sodium levels and temperature continued to be a concern after being discharged from the hospital and she required an in home nurse to do sodium checks multiple times a week through the broviac central line that had been put in while in the PICU.
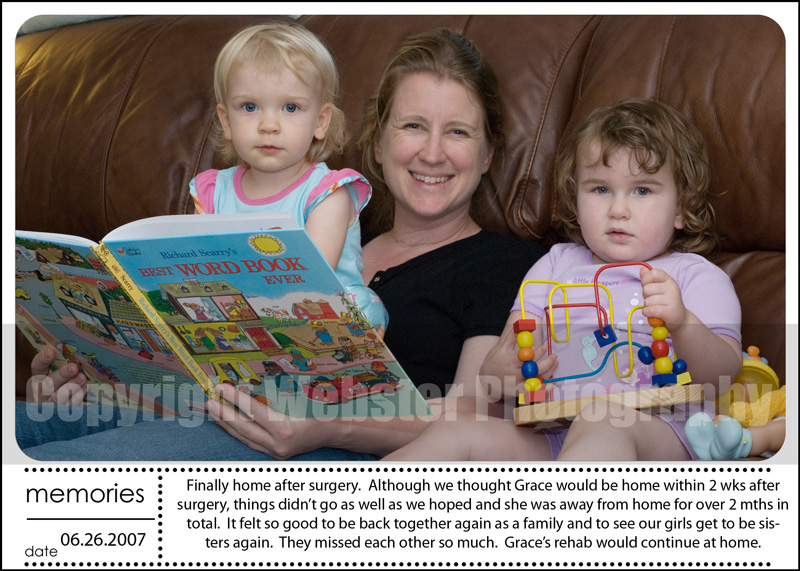
Due to the long stay in the hospital, the damage done to the hypothalamus, and the stress on her body, when Grace returned home she required continued rehabilitation. She continued to need speech therapy and occupational therapy. Due to the damage to the hypothalamus Grace’s metabolism and thyroid had been impacted, causing her to gain quite a bit of weight as well as decreased muscle strength due to the time she was pretty much bedridden.
The 60 days we lived in the two hospitals took a toll on our entire family. As a mom, I never wanted to leave Grace’s side in the hospital and in fact I only spent 1 night away from her the entire time. Every other night I was at her side. But this decision meant I had to live away from my Sarah, Grace’s younger sister. Sarah, was only 16 months when Grace had surgery. We had originally taken Sarah with us to Phoenix for Grace’s surgery, but when it became clear Grace’s post-op complications would require her to stay in the hospital, Perry and Sarah returned home to California. It was heartbreaking to have our family split between two states. We did our best to talk on the phone and to comfort both girls that our family would be back together soon.
I remember the day when Sarah made her first visit to see Grace and me at the hospital in Sacramento. It had been nearly 6 weeks since I had last seen my sweet little girl. I was amazed when I saw her walking down the hall towards Grace’s room. I barely recognized her, during the separation she got so tall and lost much of her ‘baby fat’. She looked like a little girl and not my baby from just two months earlier. The bigger surprise came when she began to ask questions about when Grace and I would be able to finally come home. My little girl had learned to talk while we were in Arizona. I wasn’t there for this huge milestone of Sarah’s and I felt like both of us had been cheated of this time together.
Grace had an MRI at six month post-op and it was reviewed by the BNI team. It was at this point that we found out the resection had been 100% and the MRI showed no hypothalamic hamartoma remaining. This was great news.
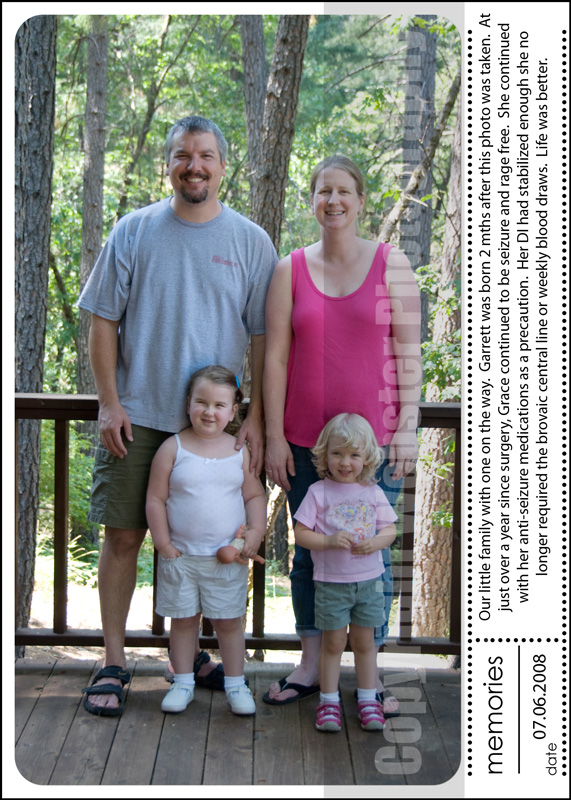
The year of recovery following surgery was tough, but the good news was Grace had not had a single seizure or a hypothalamic rage since leaving Arizona.
The post-op struggles continued with diabetes insipidus, uncontrollable hunger and a decreased metabolism. Instead of tracking seizures as we had to do before surgery, we now measured all fluids in and out, weighed her daily, measured all food and provided food on a strict time schedule. Grace’s weight gain was a constant struggle. Grace’s drive for food continued and eventually, we found she had the acquired form of Prader-Willi syndrome as a result of surgery. This was yet another devastating blow to our family and increased the care Grace required.
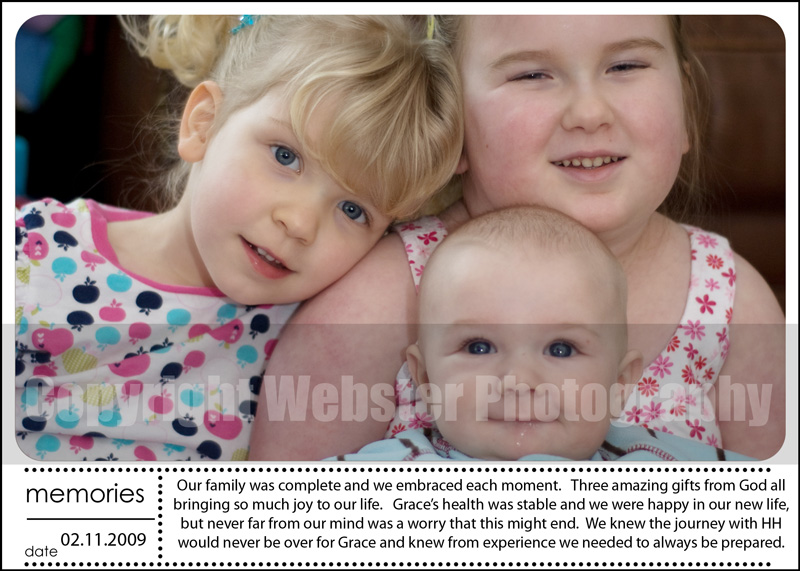
In January 2008, we found out we were expecting another addition to our family. Both girls were overjoyed with the expectation of a new baby in the house. They both loved caring for one another and had so much love to share.
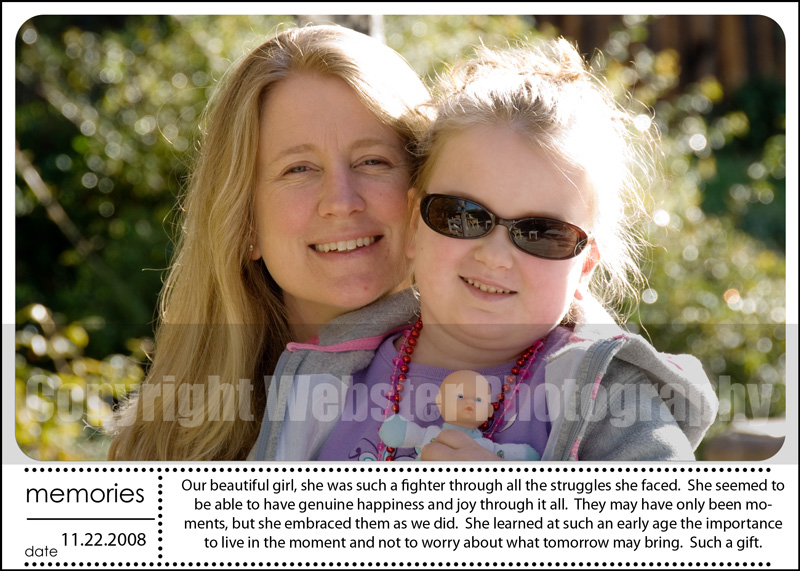
Grace started preschool in August 2008 and fell in love with it. She woke up every morning asking if it was a school day and if the answer was ‘yes’ she’d have the biggest smile. She approached each day with joy and happiness, looked forward to wearing her favorite outfit, picking her jewelry and having her hair accessories perfectly match her outfit. She loved the ‘bling’ and loved getting to school so she could show it all off to her teachers and aides. Although Grace continued to need medical monitoring of her sodium, she blossomed being around her peers.
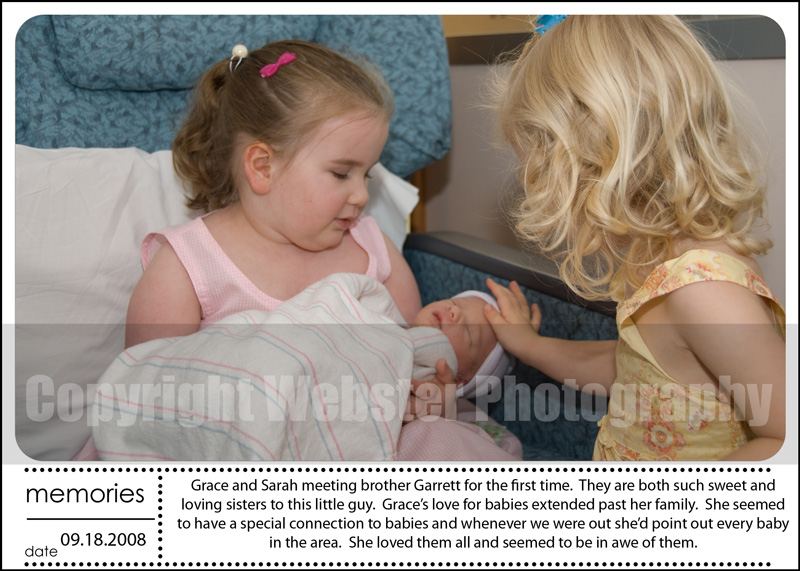
In September 2008, our family welcomed Garrett into the world. His sisters were so happy to finally get to meet him and we all knew that adding a little boy to our family was a true blessing.
Life continued to improve for Grace and in April 2009, we celebrated her two year post-op anniversary and felt blessed she continued to be seizure and rage free. She was being weaned off her anti-seizure medications slowly and life was good.
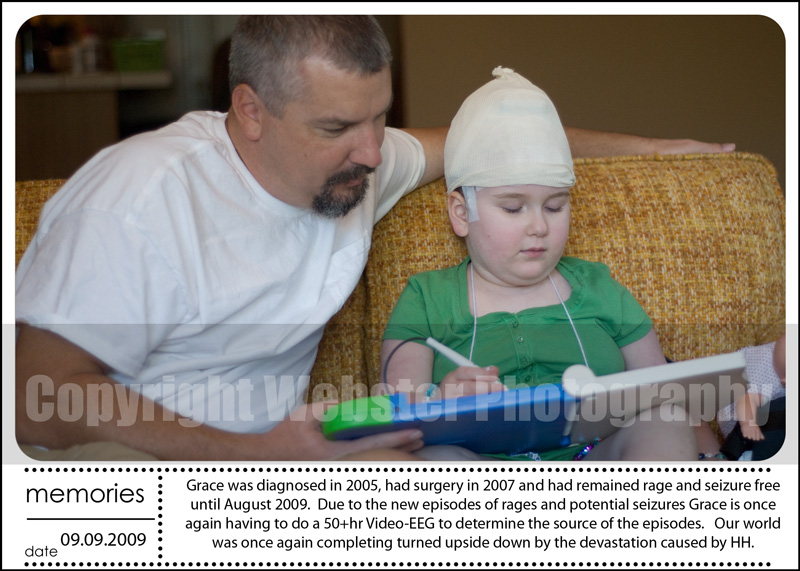
By July 2009, we began noticing ‘episodes’ of odd behaviors and blips of aggressions from Grace. These were completely out of character and we feared our world was once again going to be turned upside down. Grace was scheduled for a video-EEG and it didn’t indicate anything that would explain these ‘episodes’. However, as parents of a child with HH, we know when our children are seizing. Even though the EEG isn’t showing anything it doesn’t indicate seizures are not occurring, it simply means the seizures are localized in the center of the brain and the EEG electrodes aren’t detecting them at the surface of the scalp. The next year continued to progress with more seizures and increased aggression. Grace required 1:1 supervision at all times to ensure her safety. She became depressed and began to withdraw from life and the family she loved. We were back to a place that was worse than before surgery and felt like Grace’s life and our happiness as a family was once again being stolen by this hypothalamic hamartoma.
The next year was so reminiscent of life before surgery. We were working closely with her neurologist to find a balance of anti-seizure medications to help decrease the frequency and the progression of her seizures as well as trying to find the right anti-depressant to help with her depression. Grace’s quality of life was severely compromised during this time and our entire family was devastated at seeing her pull away from us and life. We were fortunate that her neurologist was willing to work closely with us throughout this time. I approached him regarding my theory as to her heightened level of anxiety and it being the catalyst for the increased seizures and rages, he was very open to looking at other possible solutions. When he initially recommended Prozac as a solution to the anxiety, it was a difficult thing for us to wrap our heads around. Grace was only 6.5yrs old and the thought of such a young child being on this type of medication worried us; however, we also knew that Grace’s brain did not function as that of a healthy 6.5yr old child and knew for Grace’s sake we needed to give it a try. Her happiness depended on us finding something to help her and this was the next step. Grace started Prozac in November 2010, within three days of being on the medication, the Grace that had been taken away from us in the previous year was back. Her overall anxiety level decreased dramatically and the decrease in rage behaviors was unbelievable. She began to engage in life and the things she loved. We had turned a corner and she was once again beating the odds of living with a hypthalamic hamartoma.
Life had been amazing for Grace and our family since November 2010 and 2011 will forever be remembered as the year we had our Grace back with us. She was happy. She was engaging. She was silly. She was loving. She was caring. She was loving school. She was loving playing with her siblings, Sarah and Garrett. She was the Grace that had, for so many years, been taken away from herself, as well as from our family by the devastation caused by the seizures, rages, and aggressive surgery.
In late October 2011, Grace had a routine follow up MRI, which we sent for review to the BNI team and to Dr.Rekate. We weren’t expecting the news we received. They both saw something that hadn’t been seen in the previous post-op MRIs. There was a sliver of the hypothalamic hamartoma remaining. Although unexpected news, it didn’t surprise us. Ever since Grace’s seizures and rages had reoccurred in 2009, we felt that although the doctors believed they had gotten it all, the only explanation could be that there was a small portion of the HH remaining. The doctors provided us with recommendations of treatment, including a future surgery, if that was something we wanted. Both were cautious about proceeding with a surgery as Grace’s hypothalamus had been so compromised during the first surgery and never recovered. We let them know another surgery wasn’t something we’d want to pursue and instead we were planning on heading to the epilepsy center at University of California, San Francisco, on December 14, 2011 for a consult regarding the ketogenic diet. A report earlier in the year by the team at BNI had indicated this diet may have some potential success for those with a hypothalamic hamartoma and we felt it was an opportunity for reducing or eliminating Grace’s seizures without the catastrophic risks of another surgery.
On December 11 at 2:30 am, we found Grace in her room having a seizure. The seizure was not one of Grace’s typical seizures. It was not a gelastic or a complex partial. Grace was unresponsive and this was not typical of Grace during her seizures. We knew something was terribly wrong. We called 911 and administered her clonazepam, which was for seizures lasting longer than 3-5 minutes. Grace was breathing and continued throughout the trip to the hospital. However, as soon as the ambulance pulled up to the doors, she went into cardiac arrest. Once in the ER the team brought her back, but she never regained consciousness. Her heart was weak and her body couldn’t fight anymore. Grace passed away on December 11, 2011 at 8:14am with Perry and I holding her hand and telling her how much we and her brother and sister loved her. For those few individuals who were able to get to know our Grace know how much she loved her family, how much she took care of us, and how much our happiness brought her happiness. We knew that even as her body was slipping away, our Grace was worried about us. We told her it was okay to go. We told her she had always been a fighter, but she didn’t need to fight anymore and that it was okay to go. We reassured her that we’d be okay and she didn’t need to worry about us. We told her we’d take good care of Sarah and Garrett and would always to our best to ensure their happiness. We reassured her as best as we could so that she felt free to go. She had been such a fighter her entire life and I know she fought those final hours, not for herself, but so Perry and I could have those hours with her and be able to let her know we’d be okay.
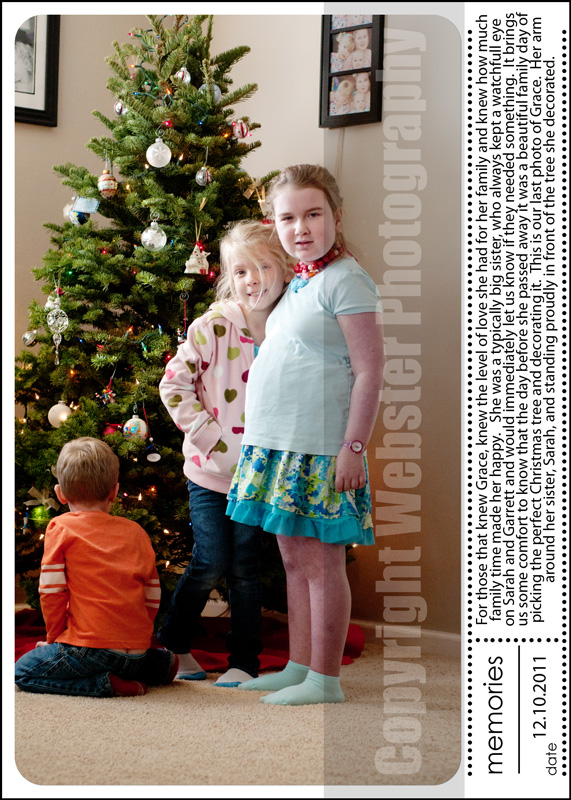
Everyone has asked, ‘How was she the night before?’ Grace was perfectly fine the day before and there was no indication she wasn’t okay. We spent the day getting a Christmas tree, decorating the tree and watching Perry put up the Christmas lights. Grace enjoyed the day and time with the family. Our last picture of Grace is her standing with her arm around her sister Sarah in front of the Christmas tree. The day before she passed was a beautiful one, with Grace doing her favorite thing. She spent the day with her family.
The specific trigger to the events that early morning will never be known. We only know for sure that Grace was having a seizure when we found her that early morning. She went into cardiac arrest and then catastrophic metabolic failure. Grace had epilepsy, precocious puberty, rages, and suffered from depression and anxiety due to the hypothalamic hamartoma. Grace had diabetes insipidus, lack of temperature regulation, hypothalamic obesity, and acquired Prader-Willi syndrome due to her damaged hypothalamus. Grace was a strong spirit, but unfortunately the body she lived with was fragile. It was only after Grace’s death did we learn about SUDEP (Sudden Unexpected Death in Epilepsy). Never once had any of her medical team mentioned this potential risk.
Grace’s medical state was complex and it was not uncommon for her to puzzle the doctors who treated her and the ER doctors were no exception. They were overwhelmed by the way her body was shutting down and believed due to lack of oxygen at some point in the events of that morning, she suffered severe brain trauma and it was the catalyst for her hypothalamus to stop working completely. Our sweet angel had struggled her entire life and on this day she returned to Heaven. We find comfort in knowing she’s no longer living with daily seizures, rages, pain, and all the other daily struggles she was inflicted with as a result of her hypothalamic tumor. She’s free from all of it.
Over the years, Perry and I had talked about Grace’s 2007 surgery. It didn’t come without a price. A price Grace suffered with everyday. She lived with more medical conditions, medications and struggles then before surgery. We know too that without that surgery Grace would have continued to have more seizures, more rages and be taken away from us both emotionally and cognitively. The surgery saved Grace. The surgery allowed us to keep our Grace on this earth a bit longer. It provided Grace the opportunity to have more true, sincere moments of joy and happiness than many individuals experience in a life time. It provided Grace the opportunity to teach her family the importance of embracing today, finding happiness in today and loving those around you today. Grace lived in the moment. She found happiness in the simple routine of her day. She wanted no more that to be at home with her family telling us ‘I love you’ each time we left her sight. So, do we regret her 2007 surgery? No, we never have or ever will regret the surgery which gave us 4.5 years longer with our Grace. Those are 4.5 years of memories we will forever cherish.
We will continue to invest our time and effort on the nonprofit, Hope For Hypothalamic Hamartomas (www.hopeforhh.org), we helped found and help spread awareness of SUDEP. Our hope is that someday the work we do here will bring about a cure to this condition. People continue to ask what they can do to help and at this time we ask only you to help us spread awareness of Grace’s condition with other friends, family and any doctors you interact with. Ask them to check out the website, ask them to donate to our cause, ask them to be aware of the risks of death as a result of epilepsy and a fragile hypothalamus.
We continue to feel blessed by the days of laughter and joy we experienced together with Grace and hold each one of them close to our hearts. From the words of our sweet Grace, ‘Have a good day’. We know she wanted that for all us while she was here and now she is wanting the same as she watches us from Heaven.
Read Grace’s Hope For HH memorial
News Articles about Grace:
Cronkite Science