Seizures in people with HH are often intractable, meaning they don’t respond well to seizure medications.
Treatment options now focus on:
- Reducing the size of the tumor or removing it if possible.
- Controlling seizures, ideally, the individual has no more seizures or at least has significantly fewer seizures.
- Stopping the decline or worsening of cognitive function.
Most doctors require individuals with HH to start their treatment plan with antiepileptic drugs (AEDs) as it is the least invasive option. In fact, some medical centers require an individual to fail a certain number of AEDs before they are considered a surgical candidate. This process can usually be completed within a relatively short period of time as most HH patients do not respond to AEDs for the control of gelastic seizures.
While some AEDs can control some types of seizures, seizure freedom or even good seizure control can be difficult to achieve for HH patients despite the use of higher doses and several combinations of antiepileptic drugs. Less than 5% of people with HH become completely seizure free with medication alone.
Gelastic seizures associated with hypothalamic hamartomas are generally resistant to medication. At this time, there does not appear to be one specific AED that is able to stop or even reduce gelastic seizures for the long term.
AEDs can however, be helpful in controlling the secondary seizures (absence, complex partial, and generalized) that
often occur with HH. The decision regarding which drugs to try first and whether to try one drug at a time, or more than one at a time, is a difficult one. Some AEDs commonly reported by HH patients include valproic acid (Depakote), levetiracetam (Keppra), lamotrigine (Lamictal), carbamazepine (Tegretol, Carbatrol), topiramate (Topamax), and oxcarbazepine (Trileptal). Also, it can take a few weeks or even months to get to an appropriate dosage of the AED to determine if its working. There are several other AEDs in use today that may also be prescribed.
Many individuals experience side effects from the drugs including cognitive impairment, fatigue, depression, drug interaction, mood swings, and loss of concentration and focus. Some individuals may experience a “honeymoon effect” where the drugs seem to be working and then lose their effectiveness for no apparent reason. Some parents have reported that their kids seem to cycle with their seizure frequency, with days or weeks of high frequency followed by days or weeks of very few seizures, regardless of medication dosage. This can lead to the belief that frequent dosage changes must be made, further complicating the treatment plan. Doctors will typically recommend adjusting dosages or stopping drugs slowly over time to minimize potential side effects.
Parents/patients should not stop or lower a seizure medication on their own – this could make seizures worse and cause long or repeated seizures called status epilepticus. Status epilepticus is said to occur when a seizure lasts too long or when seizures occur close together and the person doesn’t recover between seizures. Just like there are different types of seizures, there are also different types of status epilepticus.
When considering surgery as a treatment option, it is important to consider all the benefits and risks. Decisions about proceeding with a more invasive treatment must always be highly individualized.
For infants and young children with only gelastic seizures, the decision to “watch and wait” may be the most comfortable decision for some families.
However,it is important to understand that studies have found that 50% of children with only gelastic seizures in the early years will develop the deteriorating form of the HH syndrome (loss of developmental milestones and progressive impairment of learning and cognition) and that up to 75% to 100% will develop other seizure types in their lifetime.
Further research needs to be done comparing the outcomes of individuals who choose to intervene early versus those who delay.
All surgical approaches should be preceded by a detailed preoperative evaluation. The following tests are recommended:
- Detailed information about seizures, triggers, severity, and frequency
- The type and size of hypothalamic hamartoma
- Neuropsychological (cognitive) testing
- Neurobehavioral screening
- Endocrine (hormonal) tests
- High quality magnetic resonance imaging (MRI), using a specific HH protocol
- Electroencephalogram (EEG) monitoring, often a 24-hour video EEG may be enough to evaluate seizures. However, with HH there can be limitations to EEG results. To better understand why, read more here.
- Other imaging tests that can help look at brain function, such as fMRI, and the areas where surgery may be done.
Several successful surgical approaches are now being used which allow for complete removal or partial resection and disconnection of an HH. With the advances in surgical techniques and experience, many HH treatment centers are recommending early intervention based on quality of life comparisons. For a list of questions to ask your surgeon if you are contemplating surgery, click here.
Open Surgical approaches include:
- Transcallosal Anterior Interforniceal approach (TAIF)
- Transventricular Endoscopic Resection/Disconnection
- Orbitozygomatic Approach
Sometimes, if the first surgery doesn’t achieve the desired outcome, a second operation may be needed. The second surgical technique might be different then the first. Surgeons may also recommend a combination of approaches.
Transcallosal Anterior Interforniceal Approach
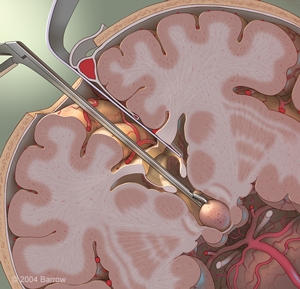
This approach is often the approach of choice for a larger hamartoma.
Most HHs are attached to one or both sides of the hypothalamus and protrude into the third ventricle, making them accessible for resection or disconnection via this approach. The main advantage of this approach is the excellent surgical view provided. A second advantage is the ability to resect (remove) and/or disconnect the HH and minimize injury to the mammillary bodies and other critically important structures that reside underneath or adjacent to the HH tumor. By approaching from above, there is less risk to the major blood vessels and cranial nerves at the base of the brain
Seizure reduction after surgery has been very promising with this approach. In addition to a reduction in seizure frequency after resection, significant improvements in behavior (with less aggression or rage), increased concentration, and improved mood have been reported.
Complications have been reported with the Transcallosal Approach. Some of the more common complications include:
- Diabetes Insipidus (DI). With DI, the kidneys are unable to conserve water and symptoms include excessive thirst and excessive urine output. DI can be successfully treated by a nasal spray (desmopressin, also known as DDAVP) administered one or more times a day. In most cases this condition resolves itself, while in some it has to be treated long term.
- Short-Term Memory deficits. The published research studies have reported that short-term memory issues are common. These resolve over time (usually days or weeks post-surgery) in most patients, but short-term memory impairment may be permanent in 10% of patients. (It is important to be aware that many HH patients have short-term memory problems even prior to surgery.)
- Increased appetite and weight gain have been reported in 10-20% of patients.
Rare problems include sleep disturbance, temperature instability, or panhypopituitarism (a deficiency in several pituitary hormones, including thyroid and growth hormone) for which replacement therapy is required.
Transventricular Endoscopic Resection/Disconnection
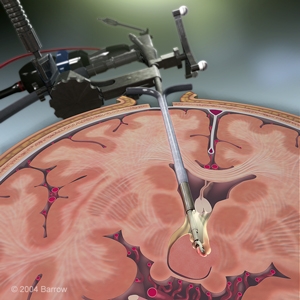
Transventricular Endoscopic Resection or disconnection has proven to be a good treatment option for smaller HHs ideally attached to only one wall of the third ventricle.
The center of the HH is removed and where possible, the interface with the hypothalamus is carefully separated. Some surgeons believe that completely disconnecting the HH from the surrounding tissue is equally as effective as surgery with complete resection or removal of the hamartoma.
Seizure reduction has been similar to the transcallosal approach and significant improvement in behavior has also been reported.
Compared to the transcallosal approach, endoscopic resection usually results in a shorter hospital stay. Surgical complications are similar to the transcallosal approach (see above).
Orbitozygomatic Approach
Before the introduction of the Transcallosal and Endoscopic approaches, resective surgery for HH was most often performed with a surgical approach from below. This approach is known as the orbitozygomatic or pterional approach.
Currently, the orbitozygomatic approach is usually restricted to HH lesions that hang down below the floor of the third ventricle. The advantage of approaching these pedunculated HH lesions from below includes a shorter distance to the HH.
For large lesions that have a base in the third ventricle but may also have a component that hangs down below the third ventricle, a combination of approaches may be required for complete resection.
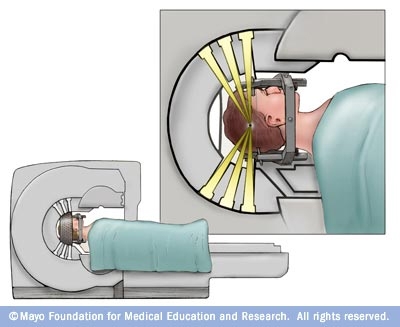
Gamma Knife Surgery (GKS) also known as stereotactic radiosurgery is a neurosurgical procedure in which high-dose radiation is targeted at the HH tumor from multiple directions, resulting in minimal radiation exposure to normal surrounding tissue. It is noninvasive (performed without opening the skull) and there is no pain or sensation from the treatment (with the exception of discomfort from the placement of a stereotactic guidance frame on the head).
Gamma Knife Surgery (GKS) has been used worldwide for other brain tumors and abnormalities and the side effects of radiosurgery are believed to be rare, transient, and in most cases very predictable. GKS is usually considered as an option for small, deeply seated lesions where there is an increased risk of complications or functional worsening with the more invasive surgeries. In these types of cases, GKS is a good first option in terms of safety, effectiveness and also cost (important to many insurance companies).
Many medical centers using Gamma Knife focus treatments on the top and sides of the hamartoma. In order to maximize effectiveness and minimize risk to the optic nerves, treatment centers will often treat the critical upper portion of the hamartoma with the higher dose while limiting the dose as it gets closer to the lower portion, closer to the optic nerve.
The advantages associated with GKS include avoiding the risks associated with surgical resection, including short-term memory problems, hypothalamic dysfunction, and bleeding.
However, a disadvantage of radiosurgery is its delayed onset of action. It is not uncommon to wait 6 months to 18 months (for some, even up to 3 years) to realize the full benefits of the treatment. For some individuals, repeat radiation may be required to get the desired effects. If GKS proves unsuccessful, standard surgery may still be an option.
For a list of questions to ask your surgeon if you are contemplating GKS surgery, click here.
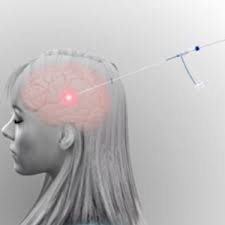
Most patients with medically refractory epilepsy and MRI-visible lesions like an HH, are potential candidates for MRI-guided laser thermal ablation therapy, also called laser ablation. This procedure may also be referred to as MR-guided laser interstitial thermal therapy or MRgLITT.
- The advantage of this technique is that surgeons can use MRI to help control and properly place a very small probe into the hypothalamic hamartoma and deliver heat to a specific area. The laser energy changes into thermal or heat energy. This can destroy the brain cells causing the seizures (commonly called seizure focus).
- Magnetic resonance imaging (MRI)is used during the procedure to monitor the heat so it targets the correct area of the brain to be “ablated”.
- A computer program marks the temperature where the probe is placed. This helps protect the brain tissue around the seizure focus.
- The heat travels a shorter distance than in other approaches.
- Treatment time and recovery time are both dramatically faster. The actual laser ablation treatment time is on the order of minutes.
- Set-up time and laser probe placement can be 3-4 hours or possibly longer in more complicated cases.
- Most patients spend one to two nights in the hospital and often are discharged the following day.
- Unlike the long waiting period for the results of the Gamma Knife Surgery, the effect of the laser is immediate.
- In the event that the procedure incompletely treats a patient’s epilepsy, repeat treatments are usually well-tolerated.
- The procedure has been proven to be effective in both children and adults.
Although thermal ablation is a minimally invasive surgery, there are some disadvantages:
- The procedure can’t be done on all lesion sizes or locations.
- It’s a new technology and we are still learning how well it can work.
- How the brain responds to heat from the laser is still not well understood.
- Some problems with memory and endocrine function have been reported after LITT. However, several studies of cognitive function after the laser procedure are better than the ones seen after open surgery.
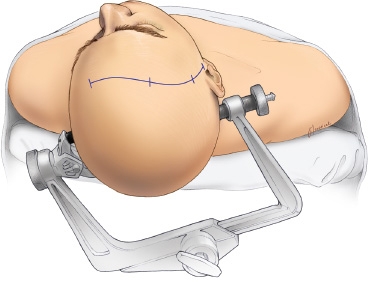
What Happens during Thermal Ablation Surgery?
- General anesthesia is still used.
- A small incision is made in the scalp, then a small hole (the size of a pencil) is made in the skull.
- An MRI is done in the operating room (or in a different room close by) to map out the exact area to be treated.
- A small (2 millimeter) tube with the laser probe is guided, using the MRI, through the small hole in the skull to the seizure focus.
- The procedure heats up and destroys the targeted area.
- A computer program checks the temperature in nearby brain areas to protect them from heat injury.
- After the procedure, the small hole in the bone and the skin incision are closed.
- Individuals usually spend just a day or two in the hospital before going home. Often the person goes back to their normal activities within 3 to 7 days.
- The most frequent side effect after the laser procedure is headache. Oral steroid medication is given for a few days to lessen swelling.
Other Resources:
- What happens during laser ablation for epilepsy? Dr. Zulma Tovar Spinoza discusses the new MRI-Guided Laser Surgery for children with brain tumors and epilepsy.
Sources:
- Curry DJ, Gowda A, McNichols RJ, Wilfong AA. MR-guided stereotactic laser ablation of epileptogenic foci in children. Epilepsy Behav. 2012 Aug;24(4):408-14.
- Hoppe C, Helmstaedter C. Laser interstitial thermotherapy (LiTT) in pediatric epilepsy surgery. Seizure. 2020 Apr;77:69-75.
- Jermakowicz WJ, Ivan ME, Cajigas I, et al. Visual Deficit From Laser Interstitial Thermal Therapy for Temporal Lobe Epilepsy: Anatomical Considerations. Oper Neurosurg (Hagerstown). 2017;13(5):627-633.
- Missios S, Bekelis K, Barnett GH. Renaissance of laser interstitial thermal ablation. Neurosurg Focus. 2015 Mar;38(3):E13.
- Tovar-Spinoza Z, Carter D, Ferrone D, Eksioglu Y, Huckins S. The use of MRI-guided laser-induced thermal ablation for epilepsy. Childs Nerv Syst. 2013 Nov;29(11):2089-94. doi: 10.1007/s00381-013-2169-6.
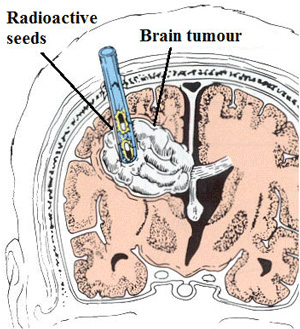
Interstitial radiosurgery involves the temporary placement of radioactive seeds into the HH tissue. These radioactive seeds emit gamma radiation with minimal delivery of harmful radiation to norma surrounding structures.
As with stereotactic thermoablation, placement of the seeds requires instrumentation into the brain, so the associated risks are still a factor to consider.
- It may take 8 weeks for a change in seizures to be seen after this procedure.
- In a study of 24 people in Germany, 38% of them were seizure free one year later and another 17% had improved significantly.
Cerebral edema (swelling), headaches, and fatigue may be seen after surgery.
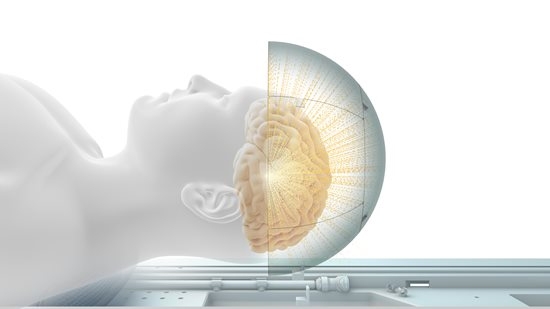
Previously studied as a treatment for other types of epilepsy, studies are being done to see how focused ultrasound can treat HH. One study at the Univeristy of Virginia is treating adults. Another at Nicklaus Children’s Hospital in Miami is testing this technique in children.
- This is a noninvasive technique, which means that an open surgery is not done.
- Concentrated ultrasound waves are used to destroy the hamartoma tissue.
- Serious side effects are not anticipated, as the technique is noninvasive.
- Since the hypothalamus produces and monitors hormones, endocrine function may be changed if normal hypothalamus tissue is affected too.
Vagus Nerve Stimulation (VNS):
In a limited number of reported cases involving VNS, most did not have much success with reducing the overall number of seizures; however, some success was reported when it came to improving rage and autistic type behaviors.
Ketogenic Diet:
The ketogenic diet has been shown in many studies to be particularly helpful for some epilepsy conditions. However, in HH the evidence is less clear. The diet works well for children with focal seizures, but may be less likely to lead to an immediate seizure-free result. It is prescribed by a physician and carefully monitored by a dietitian. If you would like to learn more about the diet click here.
Textbook Chapters
Kerrigan JF, Kahane P, Fohlen M, Arzimanoglou A. Hypothalamic hamartoma. In: Arzimanoglou A, Cross H, Gaillard WD, Holtshausen H, Jayakar P, Kahane P, Mathern G, eds. Pediatric Epilepsy Surgery. John Libbey Eurotext, Surrey, United Kingdom, 2016.
Selected Journal Articles
Du VX, Gandhi SV, Rekate HL, Mehta AD. Laser interstitial thermal therapy: a first line treatment for seizures due to hypothalamic hamartoma? Epilepsia 2017;58(Suppl 2):77-84.
Kerrigan JF, Parsons A, Tsang C, Simeone K, Coons S, Wu J. Hypothalamic hamartoma: neuropathology and epileptogenesis. Epilepsia 2017;58(Suppl 2):22-31.
Regis J, Lagmari M, Carron R, Hayashi M, McGonigal A, Daquin G, Villeneuve N, Laguitton V, Bartolomei F, Chauvel P. Safety and efficacy of Gamma Knife radiosurgery in hypothalamic hamaertomas with severe epilepsies: a prospective trial in 48 patients and review of the literature. Epilepsia 2017;58(Suppl 2):60-71.
Sonoda M, Masuda H, Shirozu H, Ito Y, Akazawa K, Asano E, Kameyama S. Predictors of cognitive function in patients with hypothalamic hamaertoma following stereotactic radiofrequency thermocoagulation surgery. Epilepsia 2017 DOI: 10.1111/epi.13838.
Harrison VS, Oatman O, Kerrigan JF. Hypothalamic hamartoma with epilepsy: review of endocrine comorbidity. Epilepsia 2017;58(suppl 2):50-59.
Hildebrand MS, Griffin NG, Damiano JA, Cops EJ, Burgess R, Ozturk E, Jones NC, Leventer RJ, Freeman JL, Harvey AS, Sadleir LG, Scheffer IE, Major H, Darbro BW, Allen AS, Goldstein DB, Kerrigan JF, Berkovic SF, Heinzen EL. Mutations of the sonic hedgehog pathway underlie hypothalamic hamartoma with gelastic epilepsy. Am J Hum Genet 2016;99:423-429.
Kameyama S, Shirozu H, Masuda H, Ito Y, Sonada M, Akezawa K. MRI-guided stereotactic radiofrequency thermocoagulation for 100 hypothalamic hamartomas. J Neurosurg 2016;124:1503-1512.
Mittal S, Mittal M, Montes JL, Farmer JP, Andermann F. Hypothalamic hamartomas. Part 1. Clinical, neuroimaging, and neurophysiological characteristics. Neurosurg Focus 2013;34(6):E6.
Mittal S, Mittal M, Montes JL, Farmer JP, Andermann F. Hypothalamic hamartomas. Part 2. Surgical considerations and outcome. Neurosurg Focus 2013;34(6):E7.
Wilfong AA, Curry DJ. Hypothalamic hamartomas: optimal approach to clinical evaluation and diagnosis. Epilepsia 2013;54(Suppl 9):109-114.
