HH and Genetics – Challenges and Opportunities
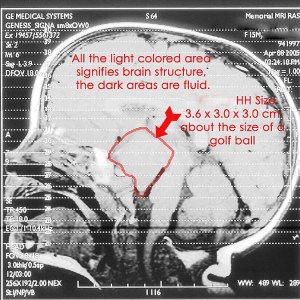
Hypothalamic hamartomas (HH) have long been described in medical literature as sporadic (random) in their occurrence, and the precise cause has yet to be determined. Sometimes, however, rather than presenting as isolated masses, HHs can be part of a multiple congenital malformation syndrome, for example – Pallister-Hall Syndrome.
These syndromes sometimes have a milder presentation and reduced impact on seizure frequency, behavior and cognitive function. However, both forms probably arise from similar mechanisms. The identification of genes associated with HH can help us better understand how to treat and diagnose as well as understand the normal development and function of the hypothalamus. Understanding the genetic component of HH has been a cornerstone of the work we continue to do as an organization. Every three years since 2013, Hope for HH has organised and hosted international conferences where we invite the world’s leading medical experts to gather and brainstorm over a couple of days. These meetings, driven by our international Medical Advisory Board, have proved invaluable in creating opportunities for collaboration, for developing global research projects, and for spearheading initiatives for our entire community’s benefit.

One of the top issues raised at the Marseille Symposium in 2013 and further discussed at the London Symposium in 2016, was a potential genetic cause of HH. Early research studies from Royal Children’s Hospital in Melbourne, Australia indicated that in some patients whose blood tests did not reveal any overall genetic abnormality, there were still some genetic abnormalities at the cellular level in the resected HH tissue itself. Drs Berkovic and Hildebrand at the University of Melbourne, initiated a project to collect and examine HH tissue, taken from patients whose HH was surgically removed, and test for potential genetic markers for HH. That collaboration has resulted in very interesting results. A full report is due to be published later this year. Unfortunately, the progress in HH surgery has led to a new challenge for researchers. The rise in the number of laser ablation surgeries has meant a reduction in HH tissue that is removed and available to study. In this hot-off-the press blog post, Dr Hildebrand explains where the research currently stands, as well as an exciting development in obtaining DNA samples from laser surgery.
An Exciting New Approach to Genetic Diagnosis of Children with HH
Authors: Dr Michael Hildebrand and Dr Samuel Berkovic, Epilepsy Research Centre, Austin Health, Department of Medicine, University of Melbourne, Victoria, Australia
We have shown when hypothalamic hamartoma tissue is available from surgery for DNA analysis a genetic diagnosis is achieved in 30-40% of children with HH 1. Due to improved and safer surgical approaches such as laser ablation we rarely get access to HH tissue for genetic analysis anymore.
A genetic diagnosis may help end the diagnostic odyssey for children with HH and their families. In the future a genetic diagnosis may also be shown to correlate with outcomes for children with HH, including seizure and developmental outcomes, but also potentially their outcomes following surgery as well. This might lead to more accurate predictions around disease course for children with HH, allowing families to better plan for the future.
To address the need to access HH tissue for genetic diagnosis we are exploring an exciting new method reported just this year by a research team led by Dr Alica Goldman at the Baylor College of Medicine in Houston 2. It turns out that even tiny amounts of brain tissue, washed off depth electrodes used to measure seizures in individuals with epilepsy undergoing evaluation for potential surgery, provides enough DNA using this new method to permit genetic analysis.
In preliminary work in Melbourne we have confirmed that it is possible to screen all of the more than 18,000 genes in our genome using tiny amounts of tissue DNA from these electrodes of an individual with focal cortical dysplasia (a different type of brain lesion to HH) and epilepsy, who was undergoing surgical evaluation.
We are now planning to trial this approach with neurosurgeons Drs Daniel Curry and Irfan Ali at Baylor College of Medicine using similarly small amounts of tissue collected from the laser probes of 5 children with HH prior to laser ablation of their tumors. Drs Curry and Ali have reported the largest cohort of children with HH who have undergone successful laser ablation surgery through their epilepsy surgery program 3,4.
If this trial is successful, it will provide an exciting new route to genetic diagnosis.
This will in turn increase the yield of genetic diagnosis for children with HH, and potentially lead to improved outcomes in management and treatment in the future.
References
- Hildebrand MS, et al. Mutations of the Sonic Hedgehog Pathway Underlie Hypothalamic Hamartoma with Gelastic Epilepsy. Am J Hum Genet 2016;99:423-9.
- Montier L, et al. A somatic mutation in MEN1 gene detected in periventricular nodular heterotopia tissue obtained from depth electrodes. Epilepsia 2019;60:e104-e9.
- Boerwinkle VL, et al. Network-targeted approach and postoperative resting-state functional MRI are associated with seizure outcome. Ann Neurol 2019;86:344-56.
- Curry DJ, et al. MR-guided laser ablation for the treatment of hypothalamic hamartomas. Epilepsy Res 2018;142:131-134.

Support Hope For HH Research Initiatives
Help ensure Hope For Hypothalamic Hamartomas can continue to host international symposiums, drive multi-center research collaborations and ensure your voice is heard by the medical community. Without your help, these initiatives would not be possible.
Learn more
International Symposium Highlights
Dr. Sam Berkovic presents an overview of Hypothalamic Hamartoma Research session
Dr. Michael S. Hildebrand presents highlights from a talk on HH Genetic Research to identify underlying mechanisms of HH
Dr. Daniel J. Curry presents a summary of his talk on the surgical technique Laser Ablation and its impact on seizures and comorbidities for HH patients





